Chemotherapy
Introduction
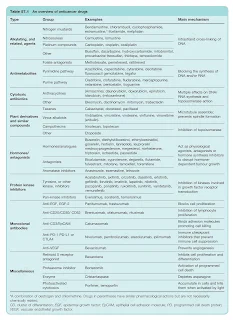
Cytotoxic drugs, along with surgery and radiotherapy, remain the mainstay of cancer treatment.
However, newer treatments based on targeting the specific malfunctions of cell cycle control that characterise cancer cells, and on increasing their susceptibility to immunological attack, are becoming increasingly important.
- These include hormone antagonists, kinase inhibitors and monoclonal antibodies.
Ministry of Health Systemic Therapy Protocol 2016
The Ministry of Health Systemic Therapy Protocol focuses on chemotherapy and targeted therapies for treating solid tumours.
- While not intended to replace international protocols, it serves as a valuable quick reference in the local setting.
For all provisional registered pharmacists, I personally recommend starting with chapters 14 and 15, which cover these essential topics:
- Pre-Chemotherapy Assessment
- Important Formulas: BSA and Calvert Formula
- Management of Emesis
- Pre-Medication for Specific Chemotherapy
- Dose Modification Guidelines
- Febrile Neutropenia
- Chemotherapy Toxicities and Management Guidelines
- Safe Handling and Administration of Cytotoxics
- Extravasation
- Cytotoxic Spill Management
- Chemotherapy Preparation and Reconstitution
After reviewing these foundational chapters, you can then read up on the specific cancer and chemotherapy protocols relevant to your hospital.
On page 77, a minor typo error regarding the EP-EMA regimen is suspected. The actinomycin D (dactinomycin) dose should be 0.5 mg per cycle as an absolute dose.
NOTE: The Ampang Protocol (e.g. v1.2012 edition) is another comprehensive guide from the Hematology Department of Ampang Hospital. It details chemotherapy protocols, treatment algorithms and management strategies for various hematological conditions.
Chemotherapy Regimens
When you first enter a cytotoxic drug reconstitution (CDR) department, chemotherapy regimens can seem like a foreign language.
- However, in reality, they are similar to managing conditions like hypertension or diabetes mellitus.
Essentially, a chemotherapy regimen is a specific protocol used to treat a particular cancer. Multidrug regimens are commonly used and are typically identified by their acronyms. For example,
- Acute Lymphoblastic Leukemia - GMALL, Hyper-CVAD, MASPORE
- Breast Cancer - FEC, FAC, Docetaxel
- Colorectal Cancer - De-grammont, Mayo, FOLFOX, FOLFIRI, XELOX
- Gestational Trophoblastic Disease - EMA-CO
- Hodgkin Lymphoma - BEACOPP, ABVD
- Multiple Myeloma - VCD
- Non-Hodgkin Lymphoma - R-CHOP
- Ovarian Cancer- Carboplatin/Paclitaxel, Cisplatin/Paclitaxel
A key drawback of traditional chemotherapy is its lacks selectivity, as it kills both cancer cells and normal, rapidly dividing cells. Consequently, patients often experience side effects such as
- Alopecia (hair loss)
- Appetite changes
- Constipation or diarrhoea
- Myelosuppression - Leading to anaemia, neutropenia, thrombocytopenia,
- Nausea and vomiting - Acute, delayed, anticipatory
- Neuropathy
- Oral mucositis
- Skin photosensitivity
- Teratogenic and temporary or permanent sterility
Chemotherapy Administration
The administration of chemotherapy is not always straightforward.
- For example, in the FEC regimen, it is recommended to administer epirubicin first, before fluorouracil and cyclophosphamide.
As a general rule, any drug known to be a vesicant should be administered first when multiple drugs are prescribed, and always after any premedication.
- This is when the integrity of the vein is at its best and the risk of extravasation is lowest.
- For practical reasons, drugs given by prolonged infusion, such as dacarbazine, should be administered last.
Common vesicants include
- Anthracyclines (e.g. daunorubicin, doxorubicin, epirubicin, idarubicin)
- Vinca alkaloids (e.g. vinblastine, vincristine, vindesine, vinorelbine)
- Dactinomycin
- Mitomycin
# For the complete list of vesicants and irritants, you may refer to Ministry of Health Systemic Therapy Protocol page 131 or Management of Chemotherapy Extravasation: ESMO Clinical Practice Guidelines, 2012.
If doxorubicin and paclitaxel must be used concomitantly, administer doxorubicin prior to paclitaxel and diligently monitor for the development of doxorubicin toxicity, such as congestive heart failure.
- Paclitaxel administration has been shown to decrease the clearance of doxorubicin (and doxorubicinol) to a clinically significant extent, resulting in increased toxicity (e.g. congestive heart failure). The mechanism of this interaction is unclear, but may be related to competition of metabolite isoenzymes (e.g. CYP3A4) or transport protein (e.g. p-glycoprotein).
- Docetaxel does not appear to share this same interaction potential, and thus may be a better therapy choice in some clinical situations.
When administered as sequential infusions, taxanes (paclitaxel, docetaxel) should be administered before platinum (cisplatin, carboplatin) to limit myelosuppression and enhance efficacy.
Additionally, only methotrexate, cytarabine and thiotepa can be given via the intrathecal route.
- Diluents for these intrathecal drugs must be preservative-free.
- Inadvertent intrathecal administration of other cytotoxics, particularly parenteral vinca alkaloids, has been known to cause death.
Summary
To manage the expectations of patients and their relatives, it is crucial to clearly inform them about the treatment goal.
Palliative chemotherapy
- Indicated for the most patients with widespread metastasis.
- To improve quality of life; survival increments are secondary.
Adjuvant chemotherapy
- To eradicate the micrometastatic disease that remains after an initial intervention that is designed to cytoreduce the tumour bulk.
- To achieve improvement in disease-free and overall survival.
Neoadjuvant chemotherapy
- Chemotherapy is administered before a planned cytoreductive therapy to
- result in a reduced requirement for surgery
- increase the likelihood of successful debulking
- reducing the duration of hospitalisation
- improve the fitness of the patient prior to interval debulking
Chemoprevention
- To prevent cancer developing in patients identified as being at particular risk.


good sharing!
ReplyDelete