Patient Care Process
Introduction
The Pharmacist's Patient Care Process (PPCP) is a fundamental, five-step framework that guides pharmacists' clinical activities.
- In 2014, the Joint Commission of Pharmacy Practitioners (JCPP), representing 11 national pharmacy organizations, endorsed the initial version of this framework.
- An updated version of the PPCP was released in 2025, expanding upon the same five core steps: Collect, Assess, Plan, Implement and Follow-up.
- This revision was made to incorporate key contemporary concepts (e.g. telehealth, electronic health records, digital health devices, clinical documentation, billing systems and independent prescribing) that reflect the evolving role of pharmacists in modern healthcare.
The Five Essential Steps
Collect
The Collect step involves gather necessary subjective and objective information to fully understand a patient's health status and needs. This data is collected and verified from multiple sources, including the patient, caregiver, observations, existing patient records and other healthcare professionals.
- Person-centered data
- This includes health concerns, priorities, goals, lifestyle factors, beliefs, preferences, cognitive and functional status, and social determinants of health that can influence health outcomes.
- Medication history
- Compile a comprehensive list of all current and past prescription and nonprescription medications and other products with potential therapeutic implications.
- Health and clinical data
- Gather all relevant medical information such as medical problems, physical assessment findings, allergies and intolerances, immunizations, vital signs, laboratory values, genomics, clinical notes, and results from clinical tests, diagnostic imaging, medical devices, and other digital health tools.
- Administrative details
- Obtain patient demographics, health insurance and contact information for other care team members, as appropriate.
Assess
During the Assess step, the pharmacist analyzes all collected information to identify and prioritize the patient's needs.
- Medication review
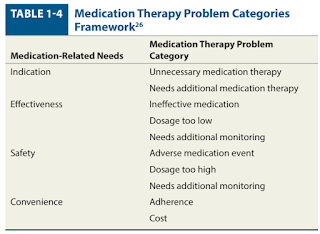
- Evaluate each medication for its indication, appropriateness, effectiveness, safety, interactions, tolerability, cost, access, convenience, and adherence to identify medication therapy problems and other medication-related needs.
- Problem identification
- Assess existing and identifying new medical problems, including diagnosing consistent with a pharmacist’s scope of practice, for potential intervention, resolution, or referral.
- Holistic evaluation
- Evaluate social determinants of health, cultural considerations, and health literacy to identify opportunities for intervention, resolution, or referral.
- Preventive care
- Determine the preventive care and wellness needs, such as medications, immunizations, education or screenings.
- Goal formulation
- Develop person-centered, evidence-based goals for the care plan.
Plan
The Plan step involves creating a person-centered, evidence-based, cost-conscious care plan in partnership with the patient and/or caregiver, and in coordination with other care team members.
- Medication optimization
- Address prioritized medication therapy problems and other medication-related needs.
- Comprehensive integration
- Incorporate prioritized medical problems, lifestyle modifications, preventive care needs, and social determinants of health into the plan.
- Care continuity
- Integrate continuity of care, safe and timely transitions of care, referrals, follow-up, and appropriate monitoring parameters.
- Shared understanding
- Confirm patient and/or caregiver understanding and agreement with the goals and plan.
Implement
In the Implement step, the pharmacist executes a prioritized care plan in partnership with the patient and/or caregiver and in coordination with other care team members.
- Therapeutic interventions
- Take action to resolve medication therapy problems and other medication-related needs by initiating, continuing, modifying, discontinuing, dispensing, administering, and/or prescribing medications consistent with scope of practice.
- Monitoring
- Order and/or perform laboratory tests and providing health monitoring tools as needed, consistent with scope of practice.
- Addressing needs
- Address prioritized medical problems, lifestyle modifications, preventive care needs, and social determinants of health.
- Education and support
- Provide the patient and/or caregiver with personalized education, a current medication list, and strategies for self-care.
- Initiate coordination of care through scheduled appointments, referrals to another care team member, and/or connection to community services.
- Documentation
- Communicate with other care team members, when needed, and documenting the care provided.
Follow Up: Monitor and Evaluate
The final step is a continuous cycle of monitoring and evaluating care plan implementation and the patient's overall health in collaboration with the patient, caregiver, and other care team members, as needed.
- Outcome assessment
- Monitor and evaluate outcomes of the care plan and progress toward achieving person-centered goals, resolving medication therapy problems and other medication-related needs, and optimizing health.
- Ongoing process
- Continue the Pharmacists' Patient Care Process for new and existing patient care needs.
The Person-Centered Approach
The person-centered approach is defined as "the practice of providing care in ways that are respectful of and responsive to individual preferences, needs, and values as well as ensuring that those receiving care or their advocates participate in decision making".
This philosophy is fundamental to the entire patient care process, as well as to practices like motivational interviewing (MI) and achieving optimal medication adherence.
- Above the evidence-based professional recommendations on disease (i.e., what generally works) lies the foundation of each patient's understanding, needs and expectations of their health, accounting for their lived realities such as financial constraints, cultural beliefs and family responsibilities.
- Without addressing these key issues, even well-informed individuals are unlikely to follow medical advice.
Knowledge and Skills
While the care process is common to all, each profession has a unique body of knowledge and skills they bring to bear when assessing the data and formulating plans.
- For pharmacy, the patient care process is focused on a patient's medication-related needs and their experience with medication therapy.
NOTE: When assessing information collected from a patient (e.g. history of present illness, physical examination, laboratory data), physicians employ a clinical reasoning process called "differential diagnosis" to weight the probability of one disease over other diseases that possibly account for the patient's signs and symptoms.
Summary
The key in the patient care process signifies the transition of the pharmacist's role from a focus on product manufacturing and dispensing to a patient-centered approach.
This patient-centered care framework can be effectively applied in any healthcare setting when providing comprehensive medication management.
- What often varies is the information collected and its source as well as the timeframe for completing the care process.
- For example, in an ambulatory care clinic, the patient is often the most important source of information. Conversely, in a critical care unit within a hospital setting, there is a greater reliance on objective data obtained through laboratory tests and diagnostic imaging studies.
External Links
- Pharmacist's Patient Care Process, 2014
- The Pharmacists’ Patient Care Process, 2025
- What is a person-led approach?, 2022

Comments
Post a Comment