Urticaria
Introduction
Urticaria is characterised by very itchy weals (hives) with or without surrounding erythematous flares.
- It may also be accompanied by angioedema.
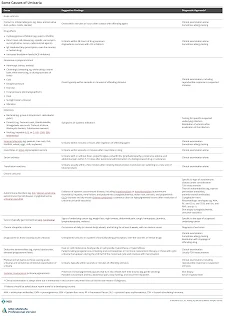
Aetiology
Urticaria can be classified according to its duration.
- Acute urticaria (<6 weeks duration)
- Often gone within hours to days.
- Most often results from type 1 hypersensitivity reactions.
- Chronic urticaria (>6 weeks duration)
- May be spontaneous or inducible.
- Most often results from idiopathic causes or autoimmune disorders.
Management
The main treatment for all forms of urticaria is with an oral second-generation H1-antihistamines.
- Second generation antihistamines are preferred because of once-daily dosing and are less sedating.
- If the standard dose is not effective, the dose can be increased up to 4-fold.
- They are stopped when the acute urticaria has settled down.
In severe acute urticaria where non-sedating antihistamines are ineffective, systemic corticosteroids (e.g. prednisolone 30 to 40 mg orally once daily) may be given short term (NOT for long term).
Intramuscular injection of adrenaline (epinephrine) is reserved for life-threatening anaphylaxis.
Identified triggers should be eliminated if possible.
- Avoid certain food or drugs.
- Cold urticaria: Dress warmly in cold or windy conditions and avoid swimming in cold water.
- Solar urticaria: Protective clothing and sunscreen application.
- Symptomatic dermographism: Reduce friction, e.g. avoid tight clothing.
For patients with chronic idiopathic urticaria who do not respond to antihistamines or other commonly used drugs, may consider omalizumab.
Summary
At a community pharmacy, you may encounter patients presenting with urticaria who seek topical treatments.
- However, there is no evidence that topical corticosteroids provide significant benefit in resolving lesions or relieving pruritus associated with urticaria.
- Oral antihistamines remain the first-line treatment and are more effective in managing symptoms.

Comments
Post a Comment